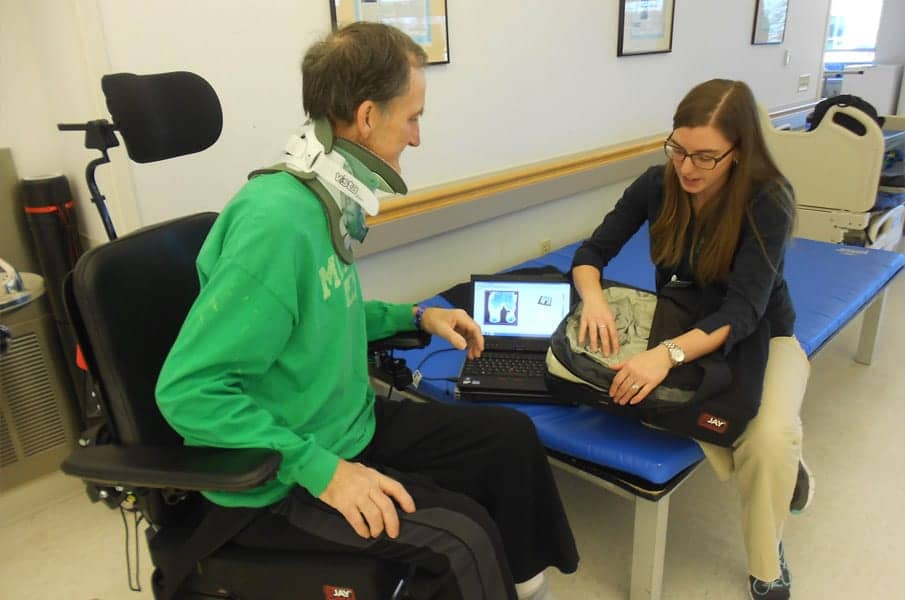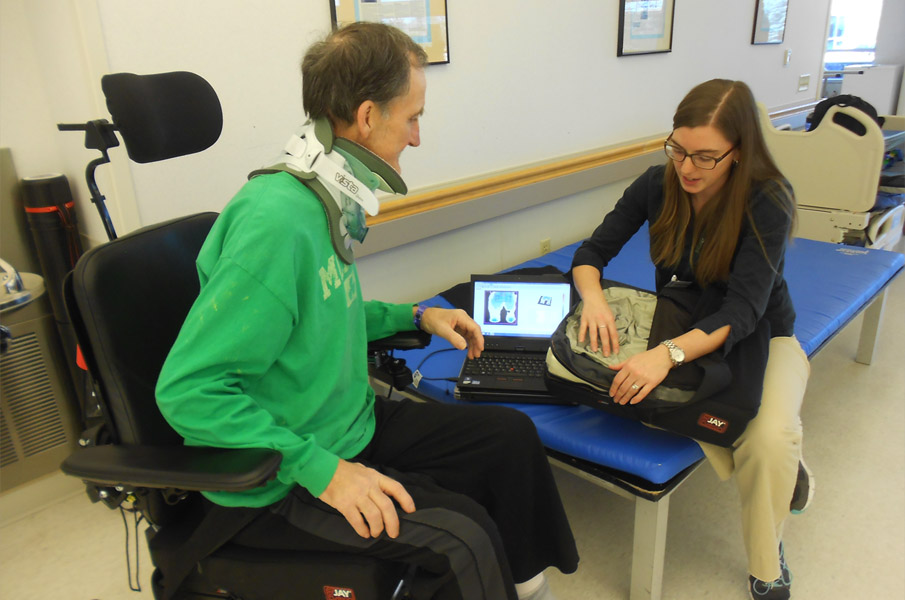
Courtney Craven, PT, DPT, provides education to a mobility device user about pressure mapping and cushion construction.
Sitting-acquired pressure ulcers (SAPUs) rank as one of the most dangerous complications that can arise for permanent wheelchair users who have suffered spinal cord injuries or have diseases of the central nervous system, The National Pressure Ulcer Advisory Panel (NPUAP) classifies pressure ulcers into four stages based on their depth from the skin surface. However, NPUAP also identifies a very severe form of pressure ulceration as deep tissue injury (DTI), defined as intact superficial skin with underlying soft tissue damage due to pressure and shear.1 DTIs appear commonly as a deep bruise but progress outward at a fast rate causing serious soft tissue necrosis and cell death in the affected region. These DTIs are costly and life-threatening, and are a topic of ongoing research to better understand their development, prevention, and treatment. Traditionally, pressure ulceration was thought to occur when pressure was applied at the superficial skin interface between a wheelchair user and their seating surface, which caused ischemia due to capillary closure with resultant cell death and breakdown. However, current literature shows that this may be too simplistic an approach, and more damaging DTIs actually develop from deep deformation of muscle and soft tissue next to bony prominences of the pelvis.2
WHEN PRESSURE AND TISSUE INTERACT
To comprehend this deep cell deformation, an understanding is necessary of the internal stresses and external forces that occur when pressure is applied to an object. Pressure itself is defined as the perpendicular force applied to a surface, and it results from contact between an individual’s bony pelvis and the seating surface as gravity pulls down the body. This causes compression of the soft tissues between the pelvis and the support surface, primarily beneath the bony ischial tuberosities and the sacrum due to their irregular shape and small dimensions. When the perpendicular pressure force is applied, parallel forces are present as well; tensile forces abnormally stretch the soft tissues, and distorting shear forces (shear stress) deform the soft tissue parallel to the applied pressure. This occurs to the greatest extent at the interface between the pelvic bony prominences and the muscle tissue directly below.3 Muscle tissue is thought to be the most sensitive to compression due to its high vascularity and metabolic demand. Consequently, pressure, combined with the distorting internal forces of tensile and shear stress, results in deformation of the muscle microstructure that can cause tissue necrosis.2
Further distortion of the compressed soft tissues occurs due to the external forces of friction and the microclimate of the region. Friction contributes to the development of shear stress by keeping the skin in place relative to movement of the person’s body during a transfer or repositioning in the wheelchair. Shear stress can then result in occlusion and disruption of blood vessels as well as loosening of connective tissue, causing reduced muscle thickness. In chronic wheelchair users, this reduced muscle thickness combined with loss of overall muscle mass can result in higher internal stresses, cell deformation, and eventual tissue necrosis. The microclimate of a region is the environment at the skin-seating interface relating to surface temperature and moisture, which can weaken the skin and increase friction to ultimately contribute to further tissue damage when pressure and shear occur.
EVALUATION AND REDISTRIBUTION
With this information creating a clearer but complex picture of pressure ulceration, the question becomes “how do we evaluate these forces, and how do they influence our decision-making in selecting a seating surface?” We first have to take into consideration how pressure is redistributed on a support surface. This depends on multiple factors, including how the body interfaces with the support surface, the mechanical and physical characteristics of both the body tissues and seating surface, and how weight is distributed in the body itself.4 Realistic expectations for ideal pressure redistribution would be low peak pressures and minimal shear forces over areas of increased risk such as bony prominences. This is accomplished through a combination of immersion and envelopment.
Immersion is defined as the depth of penetration into a support surface.5 Pressure reduction and redistribution through immersion occur as the body sinks into the support surface, increasing the surface area over which the weight is redistributed. The potential for immersion is related to the force deformation characteristics of the support surface and must be large enough to redistribute pressure away from the bony prominences. For example, in foam cushions, immersion is based on compression, but in a fluid-based cushion, it is based on displacement. Envelopment relates to the ability of a support surface to conform, in order to fit or mold around irregularities in the body.2 Concentrated areas of high peak pressures may be related to poor envelopment. Envelopment can be inhibited by the cover material of the cushion with respect to its surface tension, which, if too high, may cause a hammocking effect that produces an area of high pressure over a small contact area.3
GUIDEPOINTS FOR SEATING SURFACE AND CUSHION SELECTION
The mechanical and physical characteristics of the seating surface determine its ability to allow for immersion and envelopment. In general, seating surfaces can be broken down into two broader categories, compressive and fluid-filled.4 Compressive seating surfaces include foam (elastic and viscoelastic) and solid gel-based cushions. Fluid-filled cushions include air cell (dry flotation) and viscous fluid based cushions. Selection of a seating surface for assessment and trialing is largely based on the initial mat evaluation of the client. Obtaining a postural assessment and anatomical measurements with consideration for the client’s specific functional needs allows the clinician to select the type of cushion that meets the client’s postural and pressure redistributing needs.
Elastic foam cushions deform in proportion to load and have a tendency to return to the unloaded shape. This deformation must have a compression resistance that is high enough to support the load without creating a reactive force that increases interface pressure. Elastic foam surfaces overall have low quality immersion and envelopment, but can be improved by adding a generic contour to the foam base. However, these foams can degrade over time leading to bottoming out and high interface pressures due to loss of thickness and stiffness of the material. Viscoelastic foam cushions are made from temperature-sensitive open cell foam that is softer at operating temperatures near 98.6 degrees.1 Incorporating a layer of viscoelastic foam near the body surface can increase the quality of envelopment because it acts as a self-contouring interface. Solid gel products respond similarly to viscoelastic foam cushions.
Fluid-filled cushions are composed of cells or chambers filled with air or viscous fluid that respond to changes in pressure gradients. In general, they are capable of achieving a high degree of immersion and envelopment without large shear forces as the fluid deforms and restores. There should be an added consideration with these cushions regarding maintenance and education, as too little fluid can result in bottoming out and too much can cause high interface pressures.
Cover characteristics and materials also have an effect on friction, shear, moisture, and temperature. Covers that are made of a four-way stretch material allow for the greatest degree of immersion and envelopment as well as low shear forces, but are not very resistant to moisture and fluids. By comparison, incontinent covers are made of stiffer, moisture-resistant fabrics that serve to protect the underlying cushion materials but have higher shear forces and offer little immersion due to the increased surface tension. There is also the potential for increased risk of tissue maceration with incontinence covers due to prolonged tissue exposure to moisture that may form on the surface of the cover. Finally, microclimatic covers use a layer of spacer fabric to wick away heat and moisture while still allowing for immersion and envelopment into the seating surface.6
TRIAL AND JUDGEMENT
Once a seating surface is considered for trialing, it needs to be evaluated both subjectively and objectively to help ensure the most optimal selection for end use. The subjective reports of the client must be considered with regard to performance, function, and comfort because the client must be able to tolerate and maintain the seating surface while also utilizing it effectively in multiple environments and in the performance of multiple functional tasks. For instance, a seating surface must offer enough immersion and envelopment for optimal pressure redistribution while also affording a stable enough surface for stability and transfers. For objective assessment of the cushion and to ensure consistent comparison of pressure and shear forces, use of an interface pressure mapping system is recommended. There are a number of interface pressure mapping systems on the market. In general, these systems consist of a sensor array contained within a flexible mat that is used to measure interface pressure between the client and the support surface.7 One type of technology that can be used to look at internal shear forces is systems that use piezo resistive sensors in combination with an array of normal force sensors to measure shear forces between two forces as well as pinch shear.8
As technology and research continue to advance the understanding of how pressure and shear forces influence the development of deep tissue injuries and sitting-acquired pressure ulcers, therapists must continue to re-examine the evaluation and implementation of seating equipment and interventions. RM
Sarah Lusto, PT, MSPT, ATC, ATP, received her BS in sports medicine and MS in physical therapy from Quinnipiac University. She is a senior physical therapist on the spinal cord injury unit at the Kessler Institute for Rehabilitation in West Orange, NJ.
Courtney Craven, PT, DPT, received her BA in biology and her DPT in physical therapy from New York University. She is a senior physical therapist on the spinal cord injury and brain injury units at the Kessler Institute for Rehabilitation. For more information, contact [email protected].