Water has been a healing medium for many centuries. The unique physical properties of water make exercise easier and less painful, while increasing its effectiveness. These properties of water that make it beneficial to exercise include buoyancy, hydrostatic pressure, relative density, fluid resistance, and turbulence. Buoyancy is the force that acts in the opposite direction of gravity; hydrostatic pressure is the pressure that is exerted equally to all surface areas of an immersed body at rest at a given depth. This pressure assists the return of circulating blood to the heart, causing it to work more efficiently under less pressure; the resistance makes an individual’s muscles work harder without stressing the individual’s joints.
ON-GROUND EVALUATION
In our clinic, the initial evaluation is performed on land. The evaluation is specific to the diagnosis or area affected. Typical range of motion (ROM), strength, flexibility, and gait and balance (using the Berg Balance Test) data are obtained and may be reevaluated on land or in the water when applicable. As with land-based rehabilitation after the initial evaluation and examination, short-term and long-term goals are established. The aquatic therapist will look at the functional goals and design an aquatic rehabilitation program to best meet those goals, using the properties of water to assist when needed in providing resistance that will help achieve the rehabilitation program’s goals.
Most individuals can benefit from aquatic rehabilitation, especially those with sensory disorders, limited ROM, weakness in coordination, abnormal gait, pain (acute and chronic), spasticity, perceptual/spatial problems, balance deficits, and orthopedic injuries or trauma (including those with limited weight-bearing status and joint replacements). In addition, aquatic regimens can be therapeutic for obesity, prenatal, arthritis, fibromyalgia, osteoporosis, and neurological issues (including traumatic brain injuries, cerebral palsy, multiple sclerosis, muscular dystrophy, stroke, Parkinson’s, and post-polio syndrome). Those affected with cardiac insufficiencies and respiratory issues can also benefit from aquatic therapies.
PRECAUTIONS TO AQUATIC THERAPY
Medical clearance is required prior to initiating any exercise program, especially aquatic rehabilitation, as there are many health precautions to consider. For example, an individual’s cardiac issues can possibly be affected by hydrostatic pressure, which will change the demands of the heart while in the water or while leaving the pool. Also, pool temperatures vary from pool to pool, and can affect exercise tolerance. Although the temperature of the water is a personal preference, recommended temperatures range from 85°F to 94°F. Be cautious with any conditions that may be affected by the temperature of the water and consider recommending appropriate gear, such as a wet suit or waders, to help regulate body temperature.
Aquatic exercise is contraindicated for individuals experiencing skin infections, rashes, open wounds, sores, stitches, or contagious diseases. Aquatic exercise also should be avoided during illness (such as when suffering from a fever or a cold). Urinary tract infections or incontinence issues prohibit participation in aquatic therapies. In addition, taking medications that cause drowsiness should be avoided.
A VARIETY OF PROGRAMS
There are many different types of aquatic rehabilitation regimens that are recommended to address a variety of physical therapy needs. Among these are:
Ai Chi—a combination of deep breathing with slow movements (think of T’ai Chi in water).
Ai Chi Ne—same as Ai Chi, but it involves two participants (this is T’ai Chi with partner-assisted slow movements/stretches).
AQX—a training system designed to help individuals recover from injuries, prevent the likelihood of injuries, and increase strength, power, dynamic loading, flexibility, coordination, and endurance.
BackHab—a walking exercise program developed by aquatics authority Ruth Sova, MS, founder of the Aquatic Therapy and Rehab Institute (ATRI), West Palm Beach, Fla.
Bad Ragaz—muscle reeducation that uses specific properties of the water to progress from passive to active, isometric isotonic, and isokinetic exercise (see PNF in the Water).
Burdenko Method—focuses on vertical alignment. Builds off basic movement pattern with exercises that incorporate different planes and speeds of movements. This regimen has transition to land-based training.
Feldenkrais—a technique that is the same as that used on land to reeducate from motor learning as a baby learns to ambulate.
Halliwick—originated as a way to teach swimming to individuals with disabilities. This technique uses the properties of water and rotational patterns of human movement to increase strength, mobility, and stability, and decrease pain.
Lyu Ki Dou—uses the properties of water with the transfer of energy (translated from Japanese meaning “Floating Life Energy Pathways”).
PNF (proprioceptive neuromuscular facilitation) in the Pool—uses water to increase its benefits.
Unpredictable Command Technique—created by late aquatic expert David Ogden, PT, and used to improve somatic awareness and motor control.
Watsu—a combination of Zen Shiatsu and manipulation of a system of meridians and chakras. Based on acupuncture points with multidimensional stretching.
In addition, the benefits of standard therapeutic practices such as massage, yoga, and Pilates can be enhanced when incorporating the properties of water to the treatment.
ACCESSIBILITY
Aqua rehabilitation is available in some inpatient, outpatient, or fitness environments. Also, most sessions are individual with a one-to-one therapist to patient ratio; however, there are some group classes for those who may have been discharged from therapy and desire to continue exercising in the water.
My clinic has stairs with bilateral rails to access the pool but also has a chairlift for those who require assistance in or out of the pool. During the patient’s first aquatic session, we have a short orientation program, which includes teaching the patient pool safety such as the different depths of the pool, the effects they have, etc. Also, patients are taught how to right themselves, so that if they are working in the horizontal plane (especially with a collar), they will be able to turn over on their backs in order to breathe.
Among other safety measures to consider are keeping a waterproof phone or walkie-talkie pool side at all times.
AND THEN, THERE’S THE EQUIPMENT
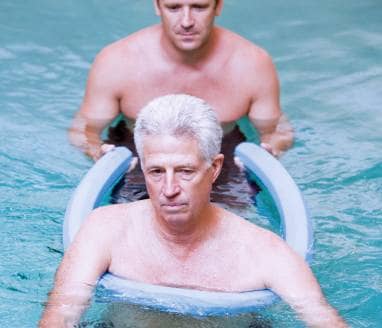
A variety of equipment can be utilized in the pool. Since buoyancy is a major property of water, most equipment is a sort of flotation aids. Examples include a flotation collar used to hold the head securely above water during exercise or flotation therapy. Flotation belts help keep the body in an upright posture to walk or jog in deep water. Foam barbells and long bar barbells could be used for flotation assistance to work on legs or as resistance aids for the upper extremities. The most common equipment used in our clinic is a pool noodle. This is because it is also the most common piece of equipment most patients have at their own pools or at community pools, which maximize the benefit of aquatic therapy when they are prescribed an individualized home exercise program.
Currently, my patient population consists mostly of patients who have been diagnosed with low back pain and/or difficulty walking or other balance problems. The benefit of water therapy allows these patients to increase their activity level safely, typically with less complaint of pain. Consider that when a patient is in waist-deep water, they will weigh about 50% of their body weight. At chest height, they will weigh 25% of their body weight. And at the top of their shoulders, just 10% of their body weight. The ability to learn to move properly with a limited amount of body weight allows these patients to increase their strength, stability, mobility, flexibility, and balance while safely decreasing their risk of falls and complaint of pain. Exercising in water allows these patients to exercise or move in a way that they would not attempt because of fear of falling, or would otherwise be unable to perform because of pain, weakness, or limited mobility. Once these patients make progress to the shallow water, there is a need to progress them to land-based exercise since we live on land and our bodies are affected by gravity on a daily basis.
Larry Jaffe, PT, DPT, SCS, ATC, a board-certified sports clinical specialist, doctor of physical therapist, and certified athletic trainer, practices at Palm Beach Aquatics and Physical Therapy in Delray Beach, Fla. For more information, contact .