(Photo above) Therapist applies DC microcurrent with a handheld device to positively influence the autonomic nervous system and accelerate the body’s healing mechanisms for a patient affected by lower back pain.
by Kelly Armstrong, OTR/L, MPP-MPS
The application of electrotherapy has been an accepted worldwide medical practice throughout the modern history of mankind. Hippocrates was reported to place patients into barrels of water with electrical eels to cure rheumatism and gout. At the turn of the 19th century, the great titans Westinghouse (direct current-DC) and Tesla (alternating current-AC) debate spawned a plethora of therapeutic electro-medical devices that flooded the market with some reportedly wild health claims. The release of the Flexner Report in 1910 wiped out the domestic electro-therapy market in favor of drugs, which remained in place until the 1960s.1
However, overseas during the 1950s, Nakatani (Japan)2 and Voll (Germany)3 actively experimented and researched low-amplitude electro-currents (microamps), both hybrid forms of electro-diagnostics and treatments. It was not until Melzack-Wall4-5 discovered the gate control theory of pain in the 1960s, (theorizing that AC electro-impulses can prevent pain sensations from traveling from injury to brain and suppressing pain), that the current domestic TENS market developed. A decade later, neuroscientist Pomeranz6-8 discovered and documented the release of beta-endorphins from the pituitary gland after both needle acupuncture and low-level DC current, unleashing the next generation of acupuncture-like TENS (AL-TENS) devices on the market.
Today, electrotherapy is being applied in Western medicine for the purpose of wound/bone healing, stress, and pain management.
How Does Electrotherapy Actually Relieve Pain?
From a biomedical prospective, all cellular activity stems from the phenomenon of electrical charge, and all healing requires a change in cellular electrical activity for success. When a muscle or tissue is injured, the injury alters the bio-electrical state of the cells, called “the current of injury.” These electrically imbalanced cells disrupt the cellular exchange process (metabolism) and negatively influence the autonomic nervous system, causing sympathetic upregulation and imbalances of the autonomic nervous system. Cellular “current of injuries” lead to loss of ATP, muscle tonicity/spasm, and chronic pain.
Therefore, to understand how electrotherapy relieves pain is to understand how electrotherapy influences imbalances of the autonomic nervous system (ANS). There are two key branches of the ANS: parasympathetic (rest and healing) and sympathetic (flight/fight/stress). It is the sympathetic system in flight/fight phase that appears to causes most health problems in humans. During SNS flight/fight phase, hormones are released and blood moves from organs to muscles to prepare for engagement. Originally designed for short-term survival, in modern society long-term nervous system stress combined with trauma often produce a lengthened and elevated state of sympathetic upregulation, resulting in chronic pain and disease. Physical traumas to the body, such as surgical scars and injuries, misalignments of the sacrum, jaw, spine, tight muscles, and blocked energetics accumulatively upregulate the SNS. One key theory in managing chronic pain and improving functionality is to learn how to deregulate the sympathetic nervous system using electrotherapy.
Electrotherapy Modalities’ Influence On the Autonomic Nervous System
Why some devices are more successful at managing pain than others may have more to do with the strength of the stimulation they produce. And, it appears, stronger is not always better.
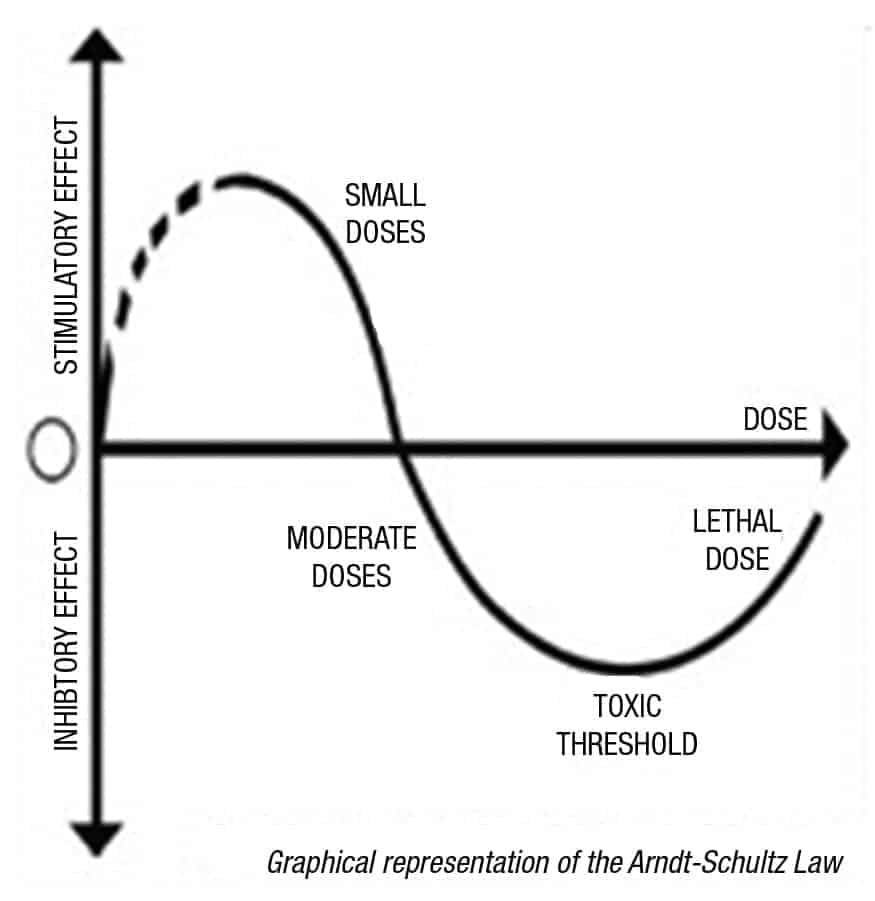
Discovered by 19th-century scientists, the “Arndt-Shultz Law” (See Figure 1) states that weak stimuli accelerates physiologic activity, and medium to strong stimuli inhibits or even halts physiologic activity.9 Applying this law to modern electro-physiology, some of the success of currents applied at low micro amperage levels is due to the ability to sympathetically deregulate the autonomic nervous system and place the patient into a self-healing parasympathetic state.
TENS: Transcutaneous electrical nerve stimulation (TENS). The United States Food and Drug Administration (FDA) classifies all electro-therapy devices as TENS, regardless of the range of electrical current applied through the skin. The traditional and popular TENS units are used as a prescription device for pain control in most clinics. Traditional TENS units are applied with AC current in the milliamperage.
TENS is usually applied at high frequency (>50 Hz) with an intensity below motor contraction (sensory intensity) or low frequency (<10 Hz) with an intensity that produces motor contraction.10-13 Frequency and amplitude of TENS produces “gate control theory of pain management,” and AC TENS has not been clinically documented to provide autonomic nervous system balance.
MENS: Microcurrent Electrical Nerve Stimulation (MENS) applies extremely small microcurrent (less than 1 milliamperage) electrical impulses to nerves using either pads or point stimulation. Microcurrent units are engineered and built to closely approximate the body’s naturally occurring bio-electric currents, and they produce electrical currents just above the levels of the electrical exchanges of the cellular level in the human body. The theory behind microcurrent therapy is that introducing micro impulses into the body restores cellular balance of positive and negative electrons, positively influencing the autonomic nervous system and accelerating the body’s own healing mechanisms.
Since microamperes are close to the electrical level of the body’s cells, when injured cells become electrically imbalanced, the application of microcurrent helps return the damaged cells to a normal bio-electrical state, re-initiating cellular activity. Research has shown that microcurrent impulses enhance three variables critical to healing: ATP (adenosine triphosphate), Protein synthesis, and Cellular Membrane transport.14-16
One detailed study by Cheng showed microcurrent applied at low levels (10 to 500 microamps) increased ATP production by 500%, protein synthesis by 70%, and metabolism (cell transport) by 40%.14-16 These three variables are critical to healing patients, and are triggered only in a parasympathetic phase. The same research documented that amplitude levels above 1 Ma inhibited ATP, protein synthesis, and cellular membrane transport, all of which are inhibited or blocked in a sympathetic state.
This documented phenomena suggests of a “sympathetic threshold” around 1 milliamperage, with current <1 Ma producing a healing parasympathetic state and current >1 Ma producing further sympathetic upregulation (See Figure 2). Is it possible the Arndt-Shultz Law theorized 200 years ago may strongly apply to electro-therapy?
EA: Electro-acupuncture (EA) is a form of acupuncture electro-therapy where a small current, either DC or AC, is applied via point stimulation directly into acupuncture/trigger points without skin puncture. Electro-acupuncture is quite similar to traditional acupuncture in that the same points are often used during treatment, just without the use of needles.17-20 One advantage EA has over traditional acupuncture is that a practitioner does not have to be as precise as with needles, since almost all devices on the market have a “point locator” which measures variances in skin resistance and “detects” acupuncture and trigger points.
EA devices fall into two categories on the market. One category is AC point stimulators, which produce current levels well into the millamperage (Ma) range and frequencies in the 10-15 hz range. The second category is DC point stimulators, which deliver an impulse in the low to medium microcurrent (50-800 mca) range, usually in the 2-4 hz range.
Additionally, EA devices can provide the benefits of integrating traditional acupuncture principles into the clinical setting. Since acupuncture has now been clinically proven to provide “a significant tool for balancing the ANS,”21-24 integrating EA into any pain setting can often provide additional outcomes to suffering patients.
Additional Beneficial Pain Modalities
LASERS: Laser technology is another noninvasive form of treatment for healing local tissues. This technology consists of using red and infrared light to irradiate abnormal tissue with photons. The cellular molecules in the tissue will absorb the energy particles. This absorption will stimulate the cell to produce more energy and to speed up the healing process. When more energy is available to cells, it stimulates healing in the body. In typical treatments the laser is placed over the injured area. There are a variety of lasers that range in wavelengths and strength of applications, with class 4 and class 3b lasers used by therapists in rehab settings as pain-relief tools.
TAPING: Therapeutic tape is an elastic cotton strip with an acrylic adhesive that is used for the purposes of treating pain and disability. Taping is a popular technique that can be applied during a clinical treatment session to facilitate healing after manual therapy. Taping may help with acute soft-tissue injuries such as muscle strains, ligament sprains, and bruising or swelling. Therapists can use taping for muscle facilitation for weak or low tone as well as to help keep joints in alignment or stable. Taping is a great tool to follow therapeutic work to assist outside of the clinic with posture. Furthermore, taping is beneficial for a variety of other issues such as bone injuries, tendinopathies, fasciopathies, systemic conditions, swelling, and edema.
TA: Topical analgesics are analgesics applied to the skin surface and associated with a lower risk of side effects than oral analgesics. There are four types of topical analgesics: counter-irritants, topical NSAIDS, capsaicin creams, and local anesthetics. Some are available as over-the-counter products, while others are available by prescription. These products may be a beneficial addition for temporary pain relief during rehabilitation. Several topical agents have been shown to be useful in short-term relief.25
Hot and cold therapy can also be of assistance in healing tissues. Application of cold packs/ice slow down the blood flood or circulation to the injured tissues and reduces inflammation, muscle spasms, and pain. Cold should be applied in the first 24 to 48 hours after an injury to decrease pain, swelling, and inflammation. Heat opens up the blood flow to the area and promotes oxygen to the tissue to relax muscles and decrease pain. Heat can also be applied during the healing process before stretching and exercises to improve range of motion.
Achieve Balance to Optimize Healing
The bottom line in helping provide pain relief is a thorough knowledge of what causes the body to heal deep inside. Key in my own practice has been cultivating an understanding that the ultimate therapeutic goal is to “swing” patients into a parasympathetic state, and to do this, the “current of injury” has to be cellularly reversed. This is an important first step that sometimes is missed.
After ANS balance, all other therapeutic techniques/modalities will be much more effective. After SNS deregulation, apply hot/cold applications and topical analgesics for acute pain and muscle relaxation, then perform your stretches/exercises with more compliance, no guarding, and better outcomes. RM
Kelly Armstrong, OTR/L, MPP-MPS, has been a practicing occupational therapist for more than 20 years, and owns a St Augustine, Fla-based private practice, Women’s Integrative Healing. She is educational coordinator at Acumed Medical as well as an author, international speaker, and instructor for pain-management seminars. Armstrong holds a bachelor of science in occupational therapy from the University of Alabama at Birmingham. For more information, contact [email protected].
References
- Flexner, Abraham (1910), Medical Education in the United States and Canada: A Report to the Carnegie Foundation for the Advancement of Teaching (PDF), Bulletin No 4, New York City: The Carnegie Foundation for the Advancement of Teaching, p. 346, OCLC 9795002
- Nakatani Y, Yamashita K. A Guide for the Application of Ryodoraku Therapy Electrical Acupuncture, a New Autonomic Nerve Regulating Therapy. EAV
- Voll R. EAV – electro-acupuncture according to Voll. Bioenergetics diagnostics and therapy on the basis of acupuncture. Voll R: Twenty Years of Electroacupuncture Diagnosis in Germany: A Progress Report. Am J Acupuncture. 1975;3(1):7-17.
- Melzack R, Wall PD. Pain Mechanisms: a New Theory. Science. 1965;150(3699):971–9. doi:10.1126/science.150.3699.971
- Melzack R, Wall PD. Pain mechanism: a new theory. Science. 1965;150:971-979
- Pomeranz B, Chin D. Naloxone blockade of acupuncture analgesia: Endorphin implicated. Life Science. 1976;19:1757-1762.
- Pomeranz B, Cheng R, Law P. Acupuncture reduces electrophysiological and behavioral responses to noxious stimuli: pituitary is implicated. Exp Neurol. 1977 Jan;54(1):172-178
- Pomeranz, B, Cheng, R. Suppression of noxious responses in single neurons of cat spinal cord by electroacupuncture and its reversal by naloxone. Experimental Neurology. 1979;64:327-341.
- Arndt-Schulz law: the pharmacologic principle of homeopathy and healing, discovered by 19th century scientists, Hugo Schulz and Rudolf Arndt, stating that weak stimuli accelerate physiologic activity, medium stimuli inhibit physiologic activity, and strong stimuli halt physiologic activity.
- Ottoson D, Lundeberg T. Pain Treatment by Tens/Transcutaneous Electrical Nerve Stimulation: A Practical Manual. Springer-Verlag; 1988.
- Sjolund B, Eriksson M. Relief of Pain by Tens: Transcutaneous Electrical Nerve Stimulation
- Chen C, Tabasam G, Johnson M. Does the pulse frequency of transcutaneous electrical nerve stimulation (TENS) influence hypo analgesia? A systematic review of studies using experimental pain and healthy human participants. Physiotherapy. 29008;94(1):11-20.
- Chesterton LS, Barlas P, Foster NE, Lundeberg T, Wright CC, Baxter GD. Sensory stimulation (TENS): effects of parameter manipulation on mechanical pain thresholds in healthy human subjects. Pain. 2002;99:253-262.
- Cheng N, Van Hoof H, Bockx E, et al. The effects of electric currents on ATP generation, protein synthesis, and membrane transport in rat skin. Clin Orthop Relat Res. 1982;171:264-272.
- Carley PJ, Wainapel SF. Electrotherapy for acceleration of wound healing: low intensity direct current. Arch Phys Med Rehabil. 1985;66(7):443-446.
- Becker RO. Cross Currents: The Perils of Electropollution, the Promise of Electromedicine. G.P. Putnam’s Sons.
- Fisher HW. Acute low back pain treated by spinal manipulation and electronic acupuncture. J Manipulative Physiol Ther. 1992;15(3):199-202.
- Cheng R, McKibbon L, Roy B, Pomeranz B. Electroacupuncture elevates blood cortisol levels in naive horses; sham treatment has no effect. Int J Neurosci. 1980;10(2-3):95-97.
- Cheng RS, Pomeranz B, Yu G. Electroacupuncture treatment of morphine-dependent mice reduces signs of withdrawal, without showing cross-tolerance. Eur J Pharmacol. 1980;68(4):477-481.
- Imai K, Ariga H, Takahashi T. Electroacupuncture improves imbalance of autonomic function under restraint stress in conscious rats. Am J Chin Med. 2009;37(1):45–55
- Noguchi E. Acupuncture regulates gut motility and secretion via nerve reflexes. Auton Neurosci. 2010;156(1-2):15-18.
- Sakatani K, Kitagawa T, Aoyama N, Sasaki M. Effects of acupuncture on autonomic nervous function and prefrontal cortex activity. Adv Exp Med Biol. 2010;662:455-460.
- Uchida S, Kagitani F, Hotta H. Neural mechanisms of reflex inhibition of heart rate elicited by acupuncture-like stimulation in anesthetized rats. Auton Neurosci. 2010;157(1-2):18–23.
- Li QQ, Shi GX, Xu Q, Wang J, Liu CZ, Wang LP. Acupuncture effect and central autonomic regulation. Evid Based Complement Alternat Med. 2013;2013:267959. doi: 10.1155/2013/267959. Epub 2013 May 26.
- Gibbs M. The role of transdermal fentanyl patches in the effective management of cancer pain. Int J Palliat Nurs. 2009;15(7):354–359.







I really like how you talk about electrotherapy relieving pain and how it works. It’s interesting how you can reach an elevated state of sympathetic upregulation. Lately, I have been getting weird pains and maybe electrotherapy would help me with that. Hopefully, I can find a product or service that can help me with this.
Hi Kelly, I’m a practicing OT in Durham, NC and would like more information about your MPP-MPS certification. Thanks for your help.
Hi Phyllis – I’ve advised Kelly about your request and asked her to respond to you here.
Hi Phyllis! I am a Master Pain Practitioner in MPS Therapy. MPS Therapy is a pain management system that is based off of eastern and western philosophies. It uses a microcurrent point stimulation device for relaxing muscles, calming the nervous system, increasing circulation, and decreasing sympathetic stress. You can read more about this integrative system at MPStherapy.com and how to become a certified pain practitioner.
can you tell me what products you offer for muscle relaxant with electrical stimulation. any help will be grateful. Mr.brazill
Hi! I use the Dolphin Neurostim device. It is a direct microcurrent device with a point application. You can purchase the device and use on injuries, scars, tight and painful muscles, and therapeutically active points. The MPS Therapy system is a pain management system that teaches protocols for chronic and acute pain and wellness. You can purchase the device and read articles and research on the DolphinNeurostim.com or MPStherapy.com websites!